Adaptation to cinnamaldehyde shapes Pseudomonas aeruginosa resistance to major antibiotics
ABSTRACT
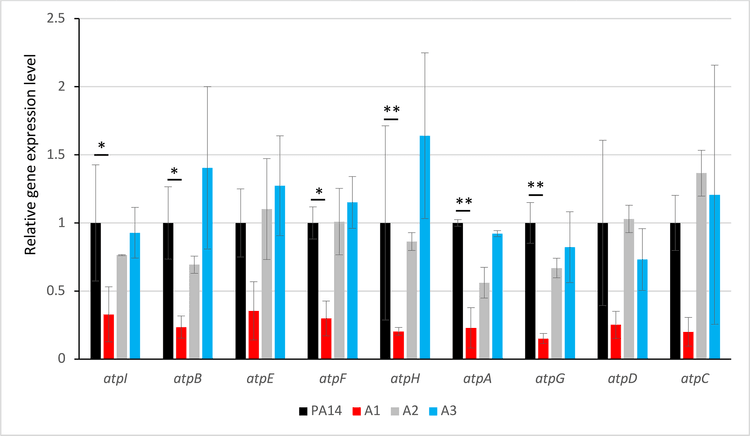
In France, the use of essential oils to treat bacterial infections is common, with approximately 40% of cystic fibrosis patients regularly using these natural products to control infections caused by Pseudomonas aeruginosa often in combination with their antibiotic treatments. Previous research has demonstrated that prolonged exposure of P. aeruginosa PA14 to cinnamaldehyde (CNA), the main component of cinnamon essential oil, can select for mutants resistant to β-lactams through overproduction of the MexAB- OprM efflux pump, some of which are also hypersusceptible to aminoglycosides and colistin. We showed here that this hypersusceptibility is not due to an efflux defect, as the deletion of MexXY(OprM)—the specific efflux pump for aminoglycosides—still results in decreased minimum inhibitory concentrations of aminoglycosides. Genome sequencing of hypersusceptible mutants revealed mutations in the ATP synthase operon or its promoter (atpIBEFHAGDC). Surprisingly, although mutations in the atp operon reduced bacterial growth and ATP production, they are not uncommon in clinical strains. We found that ATP synthase alterations modified the respiratory chain and led to inner membrane hyperpolarization, likely enhancing positively charged antibiotic (aminoglycosides and colistin) uptake and susceptibility to these molecules. In addition, the modified respiratory chain increased the proton motive force, allowing the overproduction of the MexAB-OpM efflux pump, which protects bacteria from CNA and from the clinically relevant β-lactam antibiotics. Altogether, these results indicate a trade-off between CNA resistance and aminoglycoside/colistin susceptibility, a reaction that may question the survival of P. aeruginosa in the lung of CF patients possibly submitted to these therapeutic molecules.